Introduction: The Need for Synthetic Blood
Blood transfusions have been a lifesaving medical practice for over a century, yet the world continues to face severe shortages of donor blood. The rising demand for blood transfusions due to accidents, surgeries, and chronic conditions like anemia highlights the urgent need for an alternative. Unfortunately, traditional blood donations come with numerous challenges:
- Compatibility Issues – Blood types must match to prevent dangerous immune reactions.
- Infection Risks – Despite screening, transfusions can transmit infections such as HIV and hepatitis.
- Short Shelf Life – Red blood cells only last about 42 days in storage, limiting availability.
- Limited Supply in Crisis Zones – Natural disasters and war zones often lack sufficient donor blood.
This is where synthetic blood—an engineered alternative to human blood—emerges as a promising solution. Scientists aim to develop blood substitutes that can transport oxygen effectively, last longer in storage, and be universally compatible. If successful, it could revolutionize emergency medicine, surgery, and battlefield healthcare while reducing dependency on donor blood.
What is Synthetic Blood?
Definition and Key Characteristics
Man-Made Blood , is a biologically engineered substitute designed to perform the key function of natural blood: transporting oxygen throughout the body. Unlike donor blood, which contains red and white blood cells, platelets, and plasma, Artificial Blood Substitute is a cell-free solution that mimics the oxygen-carrying ability of hemoglobin while avoiding issues like blood type mismatches, infections, and limited availability.
Key Characteristics of Bioengineered Blood
✔ Universal Compatibility – Unlike donor blood, Lab-Grown Blood does not require blood type matching, making it suitable for all patients.
✔ Longer Shelf Life – Can be stored for months or even years without refrigeration, unlike real blood, which lasts only 42 days under refrigeration.
✔ Sterile and Safe – Since it lacks living cells, Synthetic Plasma eliminates the risk of disease transmission (e.g., HIV, hepatitis) from human donors.
✔ Mass Production – Can be manufactured in large quantities, reducing dependence on human donors and alleviating global blood shortages.
✔ Rapid Oxygen Delivery – Artificial blood is designed to efficiently transport oxygen even in extreme conditions, making it ideal for trauma care, military applications, and space travel.
While Man-Made Blood is not a complete replacement for whole human blood, it serves as a life-saving alternative in emergency transfusions, combat zones, and remote medical settings where donor blood is unavailable.
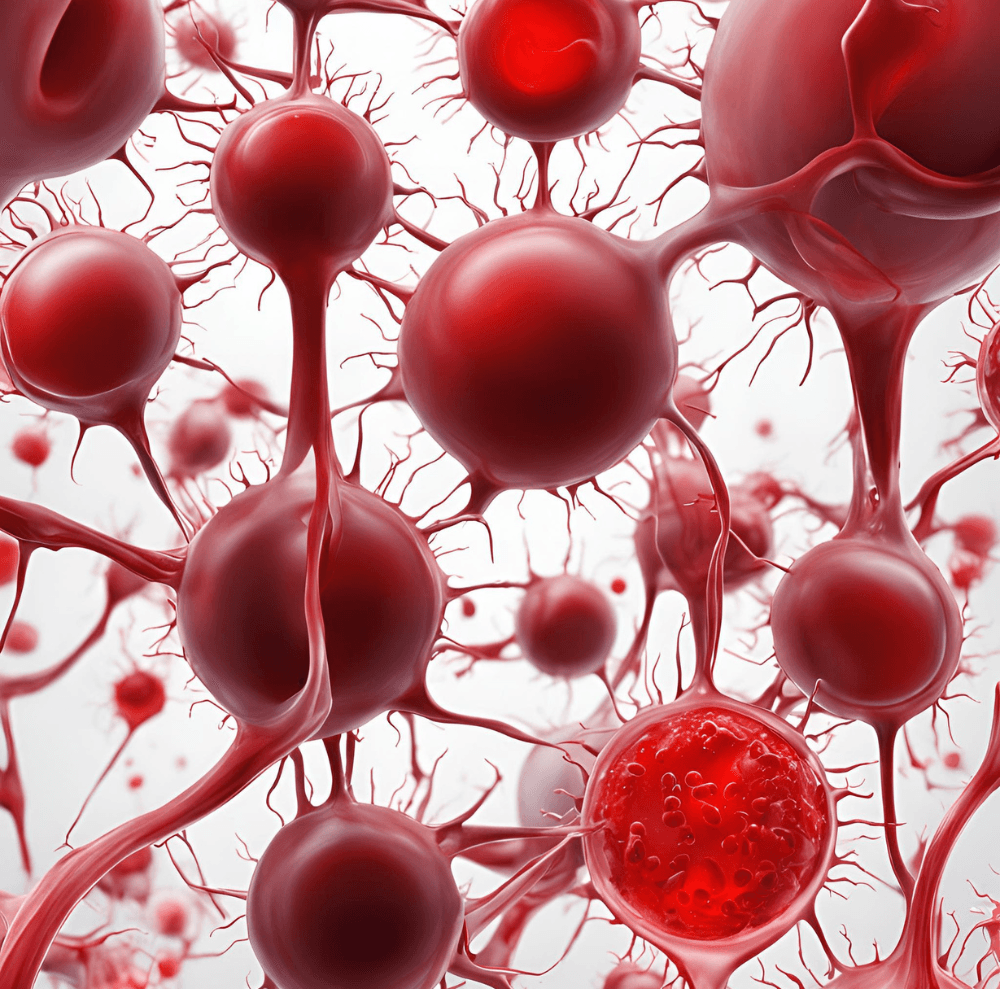
Composition and Primary Functions
Unlike natural blood, which consists of multiple components (red blood cells, white blood cells, platelets, and plasma), synthetic blood is specifically designed for oxygen transport. There are two main types of Artificial Blood Substitute:
1. Hemoglobin-Based Oxygen Carriers (HBOCs)
- Derived from human, animal, or recombinant hemoglobin, but chemically modified to enhance stability.
- Function: Directly carries and releases oxygen, similar to real hemoglobin.
- Advantages: Works immediately without requiring red blood cells.
- Limitations: May cause side effects such as increased blood pressure and oxidative stress.
- Examples: Hemopure (bovine-derived HBOC), Oxyglobin (veterinary use).
2. Perfluorocarbon-Based Emulsions (PFCs)
- Synthetic, non-biological compounds that can dissolve and transport large amounts of oxygen.
- Function: Absorbs oxygen in the lungs and releases it into tissues.
- Advantages: Completely cell-free, non-toxic, and highly stable.
- Limitations: Requires a high oxygen environment to function effectively.
- Examples: Fluosol (one of the first PFC-based blood substitutes).
How Synthetic Blood Compares to Natural Blood
| Feature | Natural Blood | Synthetic Blood |
|---|---|---|
| Composition | Cells, plasma, hemoglobin | HBOCs or PFCs |
| Oxygen Delivery | Uses hemoglobin in RBCs | Direct oxygen transport |
| Storage | 42 days (refrigerated) | Months to years |
| Risk of Infection | High (HIV, hepatitis risk) | None (sterile) |
| Availability | Donor-dependent | Mass-produced |
| Immune Response | Rejection possible | Universal compatibility |
Although Man-Made Blood does not replace platelets or immune cells, its primary role is oxygen delivery, making it a viable alternative in trauma cases, surgeries, and disaster relief efforts.
Historical Evolution and Research Milestones
The idea of blood substitutes dates back centuries, but only in recent decades has Synthetic Plasma research advanced to practical applications.
Early Attempts (17th–19th Century)
- 1667: French physician Jean-Baptiste Denys attempted the first recorded blood transfusion, using sheep’s blood in humans (with fatal results).
- 1800s: Scientists experimented with milk, saline, and other liquids as blood substitutes, but these lacked oxygen-carrying capacity.
20th Century: Early Synthetic Blood Research
- 1916: First use of anticoagulants, allowing blood storage and transfusion advancements.
- 1966: Scientists successfully tested perfluorocarbon-based (PFC) Man-Made Blood for the first time in animal studies.
- 1970s: Development of hemoglobin-based oxygen carriers (HBOCs), but early versions caused toxicity issues.
21st Century: Breakthroughs in Artificial Blood
- 1990s: Improved HBOCs such as Hemopure and Oxyglobin reached clinical trials.
- 2000s: Perfluorocarbon-based artificial blood (e.g., Fluosol) was briefly approved but later withdrawn due to low oxygen efficiency.
- 2010s–Present: Advances in nanotechnology and genetic engineering are leading to safer, more effective blood substitutes.
- 2023: Researchers developed synthetic red blood cells using nanotechnology, showing promising results in lab experiments.
Future Outlook
While fully replacing human blood remains a long-term goal, Bioengineered Blood is already proving its value in emergency medicine. Current research focuses on:
✔ Bioengineered Hemoglobin – Reducing toxicity and improving oxygen efficiency.
✔ Nanoparticle-Based Blood Substitutes – Enhancing oxygen transport with fewer side effects.
✔ Gene-Edited Synthetic Cells – Mimicking real red blood cells for longer circulation time.
Final Thoughts
Synthetic blood represents a remarkable innovation that has the potential to transform medicine. While it cannot yet fully replace natural blood, ongoing research, biotechnology, and nanomedicine advancements may soon lead to a universally available, risk-free alternative to donor blood.
How Synthetic Blood Works
How Synthetic Blood Mimics Oxygen Transport
One of the primary functions of real blood is to deliver oxygen to tissues and remove carbon dioxide, a task performed by red blood cells containing hemoglobin. Bioengineered Blood is designed to replicate this process using two main approaches:
- Hemoglobin-Based Oxygen Carriers (HBOCs) – These solutions use purified, modified, or synthetic hemoglobin to carry oxygen without requiring red blood cells.
- Perfluorocarbon-Based (PFC) Emulsions – These synthetic compounds can dissolve large amounts of oxygen and release it into tissues as needed.
Both types of Synthetic Plasma eliminate the need for blood type matching, making them ideal for emergency transfusions and battlefield medicine.
Efficiency and Shelf Life Advantages
Compared to traditional donor blood, synthetic alternatives offer several key benefits:
✔ Longer Shelf Life – Can be stored for months or even years, compared to just 42 days for real blood.
✔ No Need for Refrigeration – Some formulations remain stable at room temperature, making them ideal for remote areas and disaster zones.
✔ Higher Oxygen-Carrying Capacity – Certain synthetic formulations can deliver oxygen more efficiently than natural blood, making them valuable for patients with severe blood loss.
While Artificial Blood Substitute has yet to fully replace traditional blood transfusions, these innovations are already saving lives in experimental and emergency settings.
Blood Substitutes: The Key Players in Development
Leading Companies and Research Institutions
The development of Bioengineered Blood is being spearheaded by biotech firms, academic institutions, and government agencies, all racing to create a clinically viable, safe, and scalable blood substitute. Some of the most prominent organizations include:
Biotech Companies
- Specializes in marine invertebrate-based oxygen carriers, specifically using lugworm hemoglobin, which can transport 50 times more oxygen than human hemoglobin.
- Currently testing HemO2, a promising blood substitute with an extended shelf life and high oxygen-carrying capacity.
🔴 Sanguinate (U.S.)
- Developed an oxygenated polyethylene glycol-modified hemoglobin solution, designed to improve tissue oxygenation and reduce inflammation.
- Currently in Phase II clinical trials for treating sickle cell disease and ischemic conditions.
- Developing SpheriSome Hb, a next-generation nano-encapsulated hemoglobin-based blood substitute designed to reduce oxidative stress and blood vessel constriction.
Government & Military Research
🟢 U.S. Military Research Labs (DARPA & U.S. Army Institute of Surgical Research)
- Focused on synthetic blood solutions for battlefield medicine, aiming to develop a universal, shelf-stable blood substitute that can be used in combat zones and remote locations.
- Researching hemoglobin-based and perfluorocarbon-based artificial blood to reduce combat casualties from severe hemorrhagic shock.
🟢 Japan’s National Defense Medical College
- Working on freeze-dried Man-Made Blood, which can be easily stored and reconstituted in emergency settings.
- Their Bioengineered Blood formulation has shown success in animal trials, with human trials expected soon.
🟢 European Space Agency (ESA) & NASA
- Investigating synthetic blood substitutes for space travel, where traditional blood storage and transfusion are impractical.
- Exploring perfluorocarbon-based blood substitutes that work efficiently in low-oxygen environments.
These companies and institutions are pushing the boundaries of Bioengineered Blood research, moving toward a reliable alternative to human blood transfusions.
Notable Experimental Blood Substitutes
Several experimental blood substitutes have reached advanced clinical trials and show significant promise for real-world applications:
Hemoglobin-Based Oxygen Carriers (HBOCs)
🩸 Hemopure (Developed by Hemoglobin Oxygen Therapeutics, U.S.)
- A hemoglobin-based oxygen carrier derived from bovine hemoglobin, modified for stability and safety.
- Approved for use in South Africa for patients with severe anemia and undergoing surgery.
- Currently being tested in clinical trials for human trauma care in the U.S.
🩸 SpheriSome Hb (SpheriTech, UK)
- Uses a nano-encapsulation technology that prevents toxic free hemoglobin buildup in the bloodstream.
- Designed to mimic real red blood cells, improving oxygen delivery efficiency.
- In preclinical testing for use in trauma and emergency medicine.
Perfluorocarbon-Based Blood Substitutes (PFCs)
🩸 Oxycyte (Developed by Oxygen Biotherapeutics, U.S.)
- A perfluorocarbon-based (PFC) synthetic blood that can transport significantly more oxygen than human hemoglobin.
- Shows promise in treating traumatic brain injuries (TBI) and ischemic strokes by improving oxygen supply to damaged tissues.
- Early trials showed potential neuroprotective effects, but further research is needed for FDA approval.
🩸 Fluosol (Japan, historical development)
- One of the first FDA-approved PFC-based blood substitutes, used in the 1980s for cardiac surgery.
- Later withdrawn due to low oxygen-carrying efficiency and side effects, but paved the way for modern PFC-based Man-Made Blood.
These synthetic blood substitutes address critical medical challenges, particularly in emergency medicine, battlefield care, and chronic disease management.
Challenges in Synthetic Blood Development
Despite the tremendous progress, the widespread use of Man-Made Blood faces several major challenges:
Regulatory Approval & Safety Concerns
🛑 FDA and Global Health Approvals:
- Strict regulatory requirements demand that Bioengineered Blood undergo extensive clinical trials to prove its safety, efficacy, and long-term effects.
- Past synthetic blood substitutes faced setbacks due to side effects like vasoconstriction and organ damage.
- The U.S. FDA and European Medicines Agency (EMA) require multiple phases of trials before granting approval for human use.
🛑 Immunological Reactions & Side Effects:
- Early HBOCs caused increased blood pressure, oxidative stress, and nitric oxide depletion, leading to vascular complications.
- PFC-based substitutes sometimes require high oxygen environments, making them less effective in standard conditions.
- Researchers are working on nanotechnology-based solutions to reduce toxicity and improve stability.
Scalability & Cost Challenges
💰 Production Costs & Availability:
- Current Man-Made Blood production is expensive, with HBOCs costing over $500 per unit, compared to $150–$200 for donor blood.
- Mass production of perfluorocarbon-based substitutes remains challenging due to complex chemical synthesis.
💰 Shelf Life & Storage Issues:
- While synthetic blood lasts longer than natural blood, many current formulations still degrade over time, limiting long-term storage potential.
- Scientists are developing freeze-dried and nanoparticle-based blood that can be easily stored and reconstituted when needed.
Ethical & Public Perception Challenges
⚠️ Ethical Considerations:
- The use of animal-derived hemoglobin (e.g., from bovine sources) raises ethical concerns, particularly among vegetarian and religious communities.
- Gene-editing and synthetic biology approaches for developing artificial blood spark debates about biotech ethics and long-term risks.
⚠️ Acceptance in the Medical Community & Public Trust:
- Many doctors and hospitals hesitate to adopt Bioengineered Blood until long-term safety data is established.
- Public perception plays a huge role in adoption—patients may be reluctant to receive synthetic blood transfusions without proven long-term benefits.
Final Thoughts: The Road Ahead
Synthetic blood represents the future of transfusion medicine, with breakthroughs in biotechnology, nanomedicine, and genetic engineering paving the way for safer and more effective blood substitutes.
🔬 Key Focus Areas for Future Research:
✔ Improving oxygen transport efficiency using nanoparticles and bioengineered hemoglobin.
✔ Reducing side effects through chemical modifications and antioxidant-based formulations.
✔ Enhancing large-scale production using synthetic biology and stem cell technology.
✔ Exploring new applications such as space travel, military medicine, and organ preservation.
🚀 As technology advances, synthetic blood could soon become a mainstream, life-saving alternative—reshaping the future of medical care.
Synthetic Blood vs. Real Blood: A Comparison
Efficiency in Oxygen Delivery and Performance
Both Man-Made Blood and real blood are designed to transport oxygen, but they function differently:
- Real Blood: Uses red blood cells (RBCs) and hemoglobin to transport oxygen, requiring compatibility with the recipient’s blood type.
- Man-Made Blood: Utilizes perfluorocarbon-based (PFC) emulsions or hemoglobin-based oxygen carriers (HBOCs), allowing for immediate transfusion without blood type matching.
Performance in extreme conditions:
✔ Man-Made Blood remains stable in extreme temperatures, unlike real blood, which requires refrigeration.
✔ Synthetic alternatives offer a longer shelf life, making them ideal for disaster relief and military applications.
Immune Response, Risk Factors, and Safety
One of the biggest challenges of traditional blood transfusion is immune rejection and the risk of disease transmission.
- Real Blood Risks: May contain pathogens, require cross-matching, and can lead to immune reactions.
- Lab-Grown Blood Benefits: Is free from infectious agents and does not trigger immune rejection, reducing the risk of transfusion-related complications.
Economic and Logistical Benefits
✔ Cost-Effectiveness: Man-Made Blood reduces storage, screening, and transportation costs associated with real blood.
✔ Global Availability: Unlike donor blood, which is limited by regional shortages, synthetic blood can be mass-produced and distributed worldwide.
Potential Applications of Synthetic Blood
Emergency Medicine and Trauma Treatment
In emergency and trauma care, rapid blood loss can be fatal. Lab-Grown Blood provides:
- Immediate transfusion without cross-matching, making it ideal for accident victims, surgery, and critical care.
- Extended shelf life, allowing hospitals and ambulances to stock Lab-Grown Blood for long-term use.
Military and Space Exploration
Both the military and space agencies are investing in Bioengineered Blood research to address extreme conditions:
- Battlefield Medicine: Lab-Grown Blood can be stored at room temperature, making it an ideal solution for war zones.
- Space Missions: Space agencies like NASA are exploring Lab-Grown Blood for long-term space travel, where traditional blood storage is impractical.
Chronic Disease Treatment and Organ Transplants
Synthetic blood could play a role in treating chronic conditions and supporting organ transplants:
- Anemia Treatment: Patients with severe anemia or sickle cell disease could benefit from synthetic blood without requiring frequent transfusions.
- Organ Transplantation: Lab-Grown Blood may enhance post-transplant recovery by improving oxygen delivery to transplanted organs.
Future of Synthetic Blood & Ethical Considerations
Expected Advancements in Lab-Grown Blood Technology
The future of blood substitutes is promising, with ongoing research focusing on:
- Improved Oxygen-Carrying Efficiency: Next-generation synthetic blood will mimic natural hemoglobin more accurately.
- Biodegradable and Regenerative Alternatives: Scientists are working on artificial blood that naturally degrades and stimulates red blood cell production.
- Nanotechnology in Blood Substitutes: Researchers are exploring nano-blood carriers to enhance oxygen delivery and clotting capabilities.
Ethical Dilemmas in Human Trials and Mass Production
As with any medical breakthrough, Artificial Blood Substitute raises ethical concerns:
- Human Trials: Testing Artificial Blood Substitute on humans involves risk factors—regulatory agencies must ensure safety before large-scale use.
- Mass Production and Accessibility: Will Artificial Blood Substitute be affordable for developing nations, or will it remain a privilege of advanced healthcare systems?
- Religious and Cultural Concerns: Some communities may oppose artificial blood due to ethical, religious, or personal beliefs.
Impact on the Global Blood Donation System
With Man-Made Blood development, traditional blood donation systems may undergo transformation:
✔ Fewer Donations Needed: Reduced reliance on human donors could alleviate shortages.
✔ Healthcare Accessibility: Remote and disaster-prone areas could benefit from readily available artificial blood.
✔ Job Displacement in Blood Banks: Ethical discussions may arise over automation replacing traditional blood donation services.
Conclusion: Is Synthetic Blood the Future of Medicine?
Recap: Benefits and Challenges
Synthetic blood presents a revolutionary solution to blood shortages and infection risks, yet hurdles remain:
✅ Advantages: Longer shelf life, universal compatibility, no disease transmission.
❌ Challenges: High research costs, regulatory barriers, ethical concerns.
The Road Ahead: Research, Regulation & Commercialization
Before synthetic blood becomes mainstream, critical steps include:
- Clinical Trials & FDA Approvals: Ensuring safety, efficiency, and compatibility.
- Regulatory Frameworks: Establishing global guidelines for artificial blood production and use.
- Public Awareness & Investment: Encouraging funding and acceptance for artificial blood innovation.
The Future of Blood Substitutes: A Game-Changer?
While synthetic blood won’t replace real blood overnight, its potential for emergencies, space travel, and medicine is undeniable.
Explore our other interesting articles: