Introduction: Understanding Neuroimmunology
Neuroimmunology is an interdisciplinary field that explores the intricate relationship between the nervous and immune systems. By studying how these two complex systems interact, neuroimmunology uncovers mechanisms that regulate both health and disease. This field has significant implications for understanding conditions such as multiple sclerosis, Alzheimer’s disease, and autoimmune disorders.

The importance of neuroimmunology lies in its ability to bridge neurology and immunology—two traditionally separate domains of medicine. The nervous system communicates with the immune system through pathways such as cytokine signaling and the activation of glial cells, while the immune system can influence neurological processes like inflammation and neurodegeneration.
In modern medicine, neuroimmunology is critical because it provides insights into how to treat neurodegenerative diseases and immune-mediated disorders. It also advances the development of targeted therapies that can modulate specific neuroimmune pathways, paving the way for precision medicine in neurological care.
What Is Neuroimmunology?
Neuroimmunology is the branch of science that explores the relationship between the nervous system and the immune system. At its core, it seeks to understand how the immune system’s response can affect neural processes and vice versa.
The nervous system and immune system, though distinct in function, are interconnected in remarkable ways. The immune system, responsible for defending the body against pathogens, uses signaling molecules like cytokines to communicate with the nervous system. Similarly, the nervous system regulates immune responses through autonomic nerves and neurotransmitters. This dynamic interaction is often referred to as the neuroimmune system.
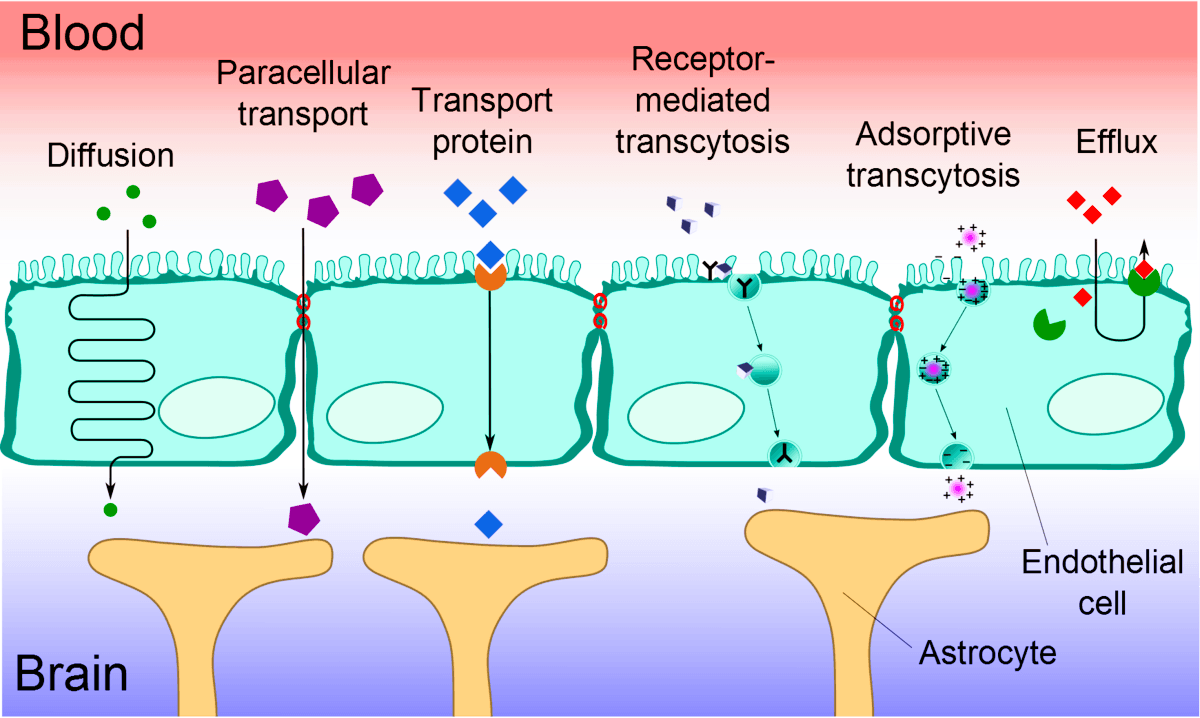
One of the foundational concepts in neuroimmunology is the role of glial cells, which support and protect neurons while also contributing to immune responses within the central nervous system (CNS). The blood-brain barrier is another critical component, as it acts as a gatekeeper, protecting the brain from harmful substances while allowing controlled immune activity.
Understanding neuroimmune pathways is essential for diagnosing and treating diseases like multiple sclerosis, where the immune system mistakenly attacks the nervous system. Moreover, studying the immune system and nervous system interactions sheds light on how inflammation can lead to neurodegenerative diseases, providing a framework for developing novel therapies.
Historical Background of Neuroimmunology
Key milestones in the development of neuroimmunology:
The evolution of neuroimmunology as a scientific field reflects a growing understanding of how the nervous and immune systems interact. The early 20th century saw the first recognition of how neurological diseases influenced the immune response. For example, Hans Selye’s work on stress in the 1930s revealed connections between the brain and immunity. By the 1960s, experiments confirmed that immune cells could cross the blood-brain barrier, traditionally thought impermeable to immune factors, initiating new discussions in the history of neuroimmunology. The 1970s marked a significant shift, as researchers identified cytokines—chemical messengers—as critical in linking these two systems.
Advancements in the evolution of neuroscience further solidified the importance of neuroimmunology. Imaging techniques, such as magnetic resonance imaging (MRI), enabled visualization of inflammation in the brain, crucial for understanding diseases like multiple sclerosis. By the 1990s, the discovery of toll-like receptors and microglial cells as immune regulators in the brain deepened insights into this dynamic interplay.
Significant discoveries shaping the field:
- Discovery of cytokines: These immune molecules act as key communicators between the brain and immune system, influencing neuroinflammation and autoimmune responses.
- Role of glial cells: Glial cells were identified as active participants in neuroimmune pathways, regulating brain inflammation and repair processes.
- Link between chronic inflammation and neurodegeneration: Studies showed that prolonged immune activation contributes to conditions such as Alzheimer’s and Parkinson’s diseases.
Role of technology and research advances:
Technological innovations have transformed the field. Advanced imaging techniques like positron emission tomography (PET) scans have made it possible to monitor inflammation in real-time. The advent of single-cell sequencing has enabled a granular understanding of neuroimmune interactions, while computational models provide new insights into how these systems co-regulate each other.
The evolution of neuroscience continues to drive progress, with modern tools such as CRISPR for gene editing and AI-powered data analysis uncovering previously unknown pathways. These advances promise earlier diagnoses and targeted therapies for neuroimmunological disorders.
Neuroimmunology Diseases and Disorders
Detailed explanation of neuroimmune-related diseases:
- Multiple Sclerosis (MS): MS is one of the most studied neuroimmunology diseases, where the immune system mistakenly attacks the protective myelin sheath of nerve fibers. This disruption leads to impaired communication between the brain and body. Symptoms include fatigue, muscle weakness, and cognitive challenges. Research on neuroinflammation has shown that cytokines and T-cells play a significant role in driving MS progression. Treatments such as monoclonal antibodies target these immune pathways.
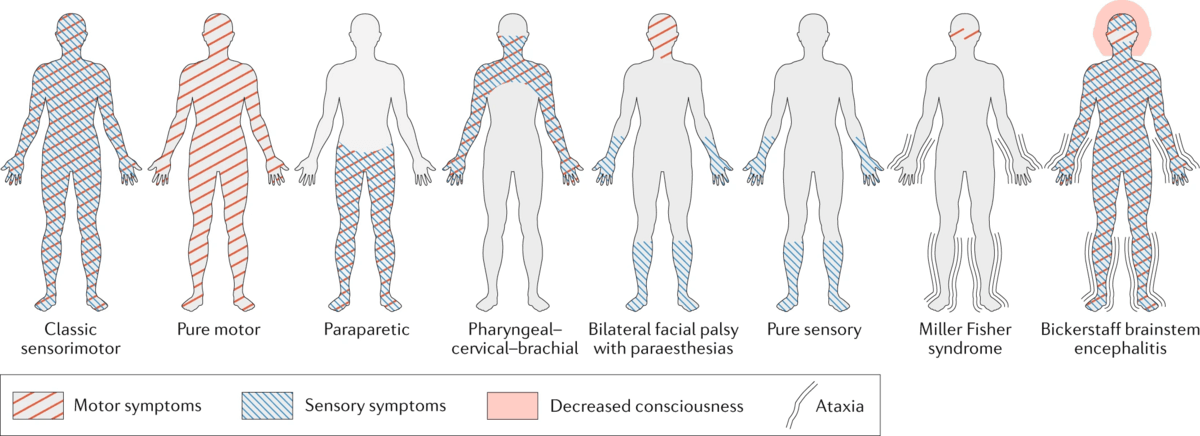
- Guillain-Barré Syndrome: A rare autoimmune disorder affecting the peripheral nervous system, Guillain-Barré Syndrome results in muscle weakness and sometimes paralysis. It often occurs following infections, with the immune system attacking peripheral nerves. This highlights the direct connection between the immune system and nervous system in triggering disorders.
- Autoimmune Encephalitis: This group of diseases involves the immune system attacking brain cells, often leading to psychiatric symptoms, seizures, and memory loss. The discovery of specific autoantibodies targeting brain receptors has improved diagnosis and treatment, bridging advances in neuroimmunology and clinical immunology.
Emerging disorders under study:
Research into the neuroimmune system has identified new conditions, including neuromyelitis optica spectrum disorder (NMOSD) and post-infectious neurological syndromes, which highlight the vast scope of neuroimmunological disorders. Conditions such as long COVID are also being investigated for their neuroimmune implications.
Challenges in diagnosing and treating these conditions:
Diagnosing neuroimmunology diseases is particularly challenging due to overlapping symptoms with other neurological or autoimmune conditions. Biomarkers such as cytokine levels or neuroimaging findings are helping refine diagnostic criteria. Treatments remain complex as they must suppress harmful immune activity without compromising the overall immune response. Emerging therapies like precision medicine and tailored immunomodulation are addressing these hurdles.
The role of neuroinflammation in these conditions:
Chronic neuroinflammation not only underpins many autoimmune disorders but also plays a critical role in neurodegenerative diseases like Alzheimer’s. Understanding the molecular pathways of neuroinflammation mechanisms, including cytokine release and blood-brain barrier disruption, is crucial for developing next-generation therapies.
The Science of Neuroimmunological Pathways
The biological mechanisms linking the immune and nervous systems:
The interplay between neurology and immunology hinges on complex biological pathways. Immune cells and signaling molecules, such as cytokines, regulate processes in the nervous system. Microglial cells, the brain’s native immune cells, serve as protectors by responding to damage and ensuring homeostasis.
The blood-brain barrier (BBB) plays a crucial role in neuroimmune regulation. Traditionally viewed as a protective shield, recent discoveries show that it selectively allows immune molecules and cells to cross, facilitating communication between the immune system and nervous system. This interaction is vital in both normal physiological processes and disease states.
The role of cytokines, glial cells, and blood-brain barrier in neuroimmune processes:
- Cytokines: These proteins act as messengers, orchestrating immune responses and mediating immune signaling in the brain. Pro-inflammatory cytokines like IL-6 and TNF-α contribute to neuroinflammation mechanisms, while anti-inflammatory cytokines regulate repair and recovery.
- Glial cells: Astrocytes and microglia are central to neuroimmune communication. Microglia respond to injury or pathogens by releasing cytokines, while astrocytes help maintain the BBB and modulate immune responses.
- Blood-brain barrier (BBB): In conditions like multiple sclerosis or encephalitis, the BBB becomes “leaky,” allowing immune cells to infiltrate the brain and exacerbate inflammation.
How neuroinflammation contributes to diseases:
Chronic neuroinflammation is a hallmark of many neuroimmunological disorders. Persistent activation of glial cells and excessive cytokine production can lead to neuronal damage. Diseases like Alzheimer’s, Parkinson’s, and multiple sclerosis have been linked to prolonged inflammation, driven by dysregulated neuroimmune pathways. Targeting these mechanisms holds promise for therapeutic breakthroughs.
Advancements in Neuroimmunology Research
Breakthroughs in understanding and targeting neuroimmune pathways:
The field of neuroimmunology has witnessed transformative breakthroughs. One key advance is the identification of biomarkers that can diagnose neuroimmune disorders early. For example, neurofilament light chain (NfL) is a biomarker for neuronal damage in conditions like multiple sclerosis.
Another breakthrough is understanding the role of microglial dysfunction in neurodegenerative diseases. This has led to therapies that aim to “retrain” these cells to restore balance in the neuroimmune system. Research into immune signaling in the brain continues to uncover pathways that can be precisely targeted.
New treatments and therapies, including monoclonal antibodies and immunomodulators:
- Monoclonal antibodies (mAbs): These engineered proteins target specific immune molecules involved in neuroimmune disorders. For example, Natalizumab is a mAb that blocks immune cell migration across the BBB, used in treating multiple sclerosis.
- Immunomodulators: Drugs like fingolimod modulate immune responses, preventing harmful inflammation without suppressing overall immunity. These therapies have revolutionized the management of neuroimmunological disorders.
Ongoing clinical trials and their potential impact:
Clinical trials are paving the way for next-generation neuroimmune therapies. Trials exploring gene-editing technologies like CRISPR aim to correct genetic defects in immune cells, while others focus on precision medicine approaches tailored to individual immune profiles.
AI-driven analysis of clinical trial data is accelerating drug discovery and refining patient selection, ensuring that treatments align with specific biomarkers. These innovations promise a future where neuroimmunology is integral to personalized medicine, improving outcomes for patients with previously untreatable conditions.
Emerging Trends in Neuroimmunology
Innovations like precision medicine in neuroimmune disorders:
The field of neuroimmunology diseases is rapidly advancing with the adoption of precision medicine, which tailors treatments to individual patients based on genetic, environmental, and lifestyle factors. This approach is particularly transformative for neuroimmunological disorders, where patient-specific variability often influences disease progression and response to therapies. By identifying neuroimmune biomarkers, such as cytokine profiles and genetic mutations, researchers can develop therapies that target specific neuroimmune pathways more effectively. For example, targeting specific interleukins in multiple sclerosis or autoimmune encephalitis is showing promising results.
Use of AI and big data in studying neuroimmune connections:
Artificial Intelligence (AI) and big data analytics are revolutionizing the understanding of the neuroimmune interface. Machine learning algorithms are being used to analyze large datasets of patient information, including genomics, proteomics, and clinical records. These tools help identify patterns in neuroimmune interactions, offering insights into disease mechanisms and potential therapeutic targets. Predictive models powered by AI are also aiding in early diagnosis by detecting subtle immune and nervous system changes that precede clinical symptoms.

Predictive models for disease progression and patient-specific treatments:
With advancements in AI, predictive models are becoming more accurate in forecasting disease progression in patients with neuroimmunological disorders. These models integrate data from imaging studies, biomarker analyses, and clinical observations to provide real-time assessments of disease trajectories. For example, in diseases like multiple sclerosis, predictive tools can inform treatment decisions by identifying patients at high risk of relapse or severe progression. By combining these models with precision medicine, clinicians can offer patient-specific interventions, minimizing side effects and improving outcomes.
Future Perspectives
What lies ahead for neuroimmunology as a field:
The future of neuroimmunology is poised to bring groundbreaking changes to medicine and science. With ongoing discoveries in the brain-immune connection, researchers aim to decode the intricate signaling networks that govern neuroimmune interactions. The integration of multi-omics technologies, such as genomics, proteomics, and metabolomics, will provide deeper insights into disease mechanisms and open new avenues for targeted therapies.
The potential for curative therapies in neuroimmunological diseases:
Emerging therapies, including gene editing tools like CRISPR, are being explored to correct underlying genetic defects in neuroimmunological disorders. Advances in regenerative medicine and neuroimmune therapies hold the promise of reversing disease damage, especially in conditions like autoimmune encephalitis and chronic neuroinflammation. Clinical trials are underway for therapies aimed at completely halting disease progression, a significant step toward achieving curative outcomes.
Broader implications for public health and personalized medicine:
As the field advances, the implications extend beyond individual treatments to global public health strategies. Early detection of neuroimmunology diseases through accessible biomarker testing can reduce healthcare burdens by preventing severe disease stages. Personalized medicine approaches, driven by advancements in integrative medicine, will likely transform healthcare delivery by offering holistic, patient-centered solutions.
Conclusion
What is neuroimmunology? At its core, it is the study of the intricate relationships between the immune and nervous systems, unraveling how these interactions contribute to health and disease. The understanding of neuroimmunological disorders has shed light on conditions once considered untreatable, offering hope to millions of patients.
The study of the brain-immune connection has positioned neuroimmunology as a cornerstone of modern medicine. From identifying disease-specific biomarkers to developing advanced therapies, this field is shaping the future of healthcare. As innovations continue, its integration into routine clinical practice will revolutionize how we prevent, diagnose, and treat complex disorders, reaffirming its vital role in scientific and medical progress.
Further Reading
Expand your knowledge on related topics by exploring the following articles:
- The Evolution of Diagnostic Imaging: A Historical Overview
Delve into the fascinating journey of diagnostic imaging, from early X-rays to modern MRI and CT scans, and discover how these advancements have transformed healthcare. - The History of Medtech: Transformations in Medical Technology
Explore the timeline of medical technology, highlighting key innovations that revolutionized diagnostics, treatment, and patient care. - How Augmented Reality is Revolutionizing Healthcare
Learn about the role of augmented reality in enhancing medical training, surgical precision, and patient experience in today’s healthcare landscape.