Introduction to Optogenetics in Humans
Optogenetics is a groundbreaking intersection of optics and genetics, offering an innovative way to control the activity of neurons with unprecedented precision. By leveraging light-sensitive proteins known as opsins, optogenetics allows for the precise activation or inhibition of specific neurons. This technology has radically transformed neuroscience, enabling researchers to map neural circuits, investigate brain disorders, and explore how neuronal communication underpins behavior.
Optogenetics works by introducing light-sensitive proteins into neurons. The most well-known of these proteins are channelrhodopsins, which are derived from algae and respond to specific wavelengths of light. Once neurons express these opsins, they can be manipulated with light pulses to either trigger or halt electrical activity, depending on the opsin used. This level of precision, coupled with the ability to control neural circuits in real time, makes optogenetics a highly valuable tool for studying brain function and behavior.

Optogenetics has achieved several notable breakthroughs since its development in the early 2000s. Researchers have used this technology to modulate neural activity in animal models, providing valuable insights into conditions such as depression, epilepsy, and Parkinson’s disease. A major leap forward was the successful restoration of visual function in blind mice, which demonstrated the therapeutic potential of optogenetics therapy for humans. These achievements have raised excitement about the future of optogenetics in humans, as researchers explore its potential to treat various neurological disorders.
The significance of optogenetics extends beyond research; it has also opened the door to new therapeutic applications, particularly in the field of neurology. By manipulating specific neurons responsible for motor control, memory, or sensory perception, optogenetics could potentially revolutionize how we treat complex brain disorders. This blog provides a detailed optogenetic review, focusing on the potential of this technology for human applications, its challenges, and its future prospects.
Optogenetics in Humans: Current State
While optogenetics has revolutionized research in animal models, the question remains: How close are we to applying optogenetics in humans? Scientists are actively investigating the use of optogenetics therapy to treat human neurological disorders, including vision restoration and Parkinson’s disease. The results thus far are promising, but significant challenges remain before optogenetics can become a mainstream therapeutic option.
One of the most exciting applications of optogenetics in humans is the potential for vision restoration. Patients suffering from retinal degenerative diseases such as retinitis pigmentosa or age-related macular degeneration could benefit greatly from optogenetic therapies. These conditions damage the photoreceptors in the retina, leading to vision loss. However, by introducing light-sensitive opsins into the remaining retinal cells, researchers can restore the eye’s ability to perceive light. In animal models, this approach has shown promising results, with mice and primates regaining partial vision. Optogenetics therapy for vision restoration is now being tested in early human trials, with the hope of providing a breakthrough treatment for millions of people suffering from visual impairments.
Another area of active research is Parkinson’s disease, a degenerative disorder of the central nervous system that affects movement. The disease is caused by the death of dopamine-producing neurons in a specific area of the brain called the substantia nigra. Current treatments, such as deep brain stimulation, provide some relief from symptoms but do not address the root cause of the disease. Optogenetics therapy offers a more targeted approach, allowing researchers to precisely control the activity of specific brain circuits involved in movement regulation. By introducing channelrhodopsins into dopamine-producing neurons, researchers have been able to alleviate motor symptoms in animal models of Parkinson’s disease. The hope is that similar approaches could eventually be used in humans.
Delivering opsins to human neurons presents its own set of challenges. Viral vectors such as adeno-associated viruses (AAV) and lentiviruses are currently the most common methods for introducing opsins into neurons. These vectors are engineered to carry the genetic material needed to express opsins in the target cells. In human applications, AAV is particularly favored due to its relatively low immunogenicity and long-lasting expression in neurons. Lentiviruses are also used, particularly in cases where larger genetic payloads are required. However, ensuring that these viral vectors are safe and effective in humans is a critical step in developing optogenetics therapy.
The potential benefits of optogenetics in humans are substantial. In addition to vision restoration and the treatment of movement disorders, optogenetics could be used to treat a wide range of neurological conditions, including epilepsy, depression, and chronic pain. The ability to precisely control neural activity could provide a more effective and targeted treatment than current pharmacological or surgical interventions.
The Challenges of Human Application
Despite its promise, several barriers must be overcome before optogenetics can be widely used in human medicine. One of the primary challenges is the technical difficulty of delivering opsins to human neurons safely and effectively. While viral vectors such as AAV and lentiviruses have been used successfully in animal models, there is still much to learn about their long-term effects on human tissues. The introduction of foreign genes into the brain, even for therapeutic purposes, raises concerns about potential immune responses, the risk of tumor formation, and other unintended consequences.
In addition to the technical challenges, there are significant ethical concerns surrounding the use of optogenetics in humans. One of the primary ethical questions relates to the genetic modification of human cells. While optogenetics offers a powerful new tool for treating neurological disorders, it also involves altering the genetic makeup of patients’ cells. This raises questions about the long-term impact of such modifications, both for the individual patient and for future generations.
Another ethical concern is the use of implantable devices to deliver light to the brain. For optogenetics to work in humans, light must be delivered directly to the optogenetically-modified neurons. This typically requires the use of invasive devices, such as fiber-optic cables or LED arrays, which are implanted into the brain. The long-term safety of these devices is still under investigation, and there are concerns about the potential for infection, device failure, and other complications.
Current clinical trials for optogenetics therapy in humans are addressing these challenges, but progress has been slow. While early trials for vision restoration are underway, it will likely be several more years before optogenetics is widely used in human medicine. Researchers must balance the need for thorough safety testing with the urgency of finding new treatments for patients suffering from debilitating neurological disorders.
The Role of Channelrhodopsin and Other Opsins in Therapy
At the heart of optogenetics therapy are opsins, the light-sensitive proteins that make this technology possible. Optogenetics channelrhodopsin, in particular, has played a central role in the development of this field. Channelrhodopsins are a type of opsin that, when exposed to light, open ion channels in the cell membrane. This causes a change in the electrical properties of the neuron, triggering or inhibiting the firing of action potentials. This process allows researchers to control the activity of specific neurons with incredible precision.
Optogenetics channelrhodopsin has been widely used in animal models to study the neural circuits underlying behavior and disease. By selectively activating or inhibiting neurons, researchers can map the pathways involved in processes such as movement, memory, and sensory perception. In addition to channelrhodopsins, other opsins have been developed to provide even greater control over neural activity. For example, halorhodopsins are opsins that respond to light by inhibiting neuronal firing, allowing for the suppression of specific neural circuits.
The development of more efficient and versatile opsins has been a major focus of optogenetic research. Scientists are working to design opsins that are better suited for use in humans, with improved light sensitivity, faster response times, and greater specificity for target neurons. These advances are essential for the successful application of optogenetics in humans, as they will allow for more precise control of neural activity in therapeutic settings.
The ability to selectively activate or inhibit neurons with light offers a powerful new approach to treating neurological disorders. In the future, optogenetics channelrhodopsin and other opsins could be used to restore lost functions, alleviate symptoms of neurodegenerative diseases, or even modify behavior. However, much work remains to be done to translate these promising findings into clinical applications.
Optogenetic Devices: From Rodents to Humans
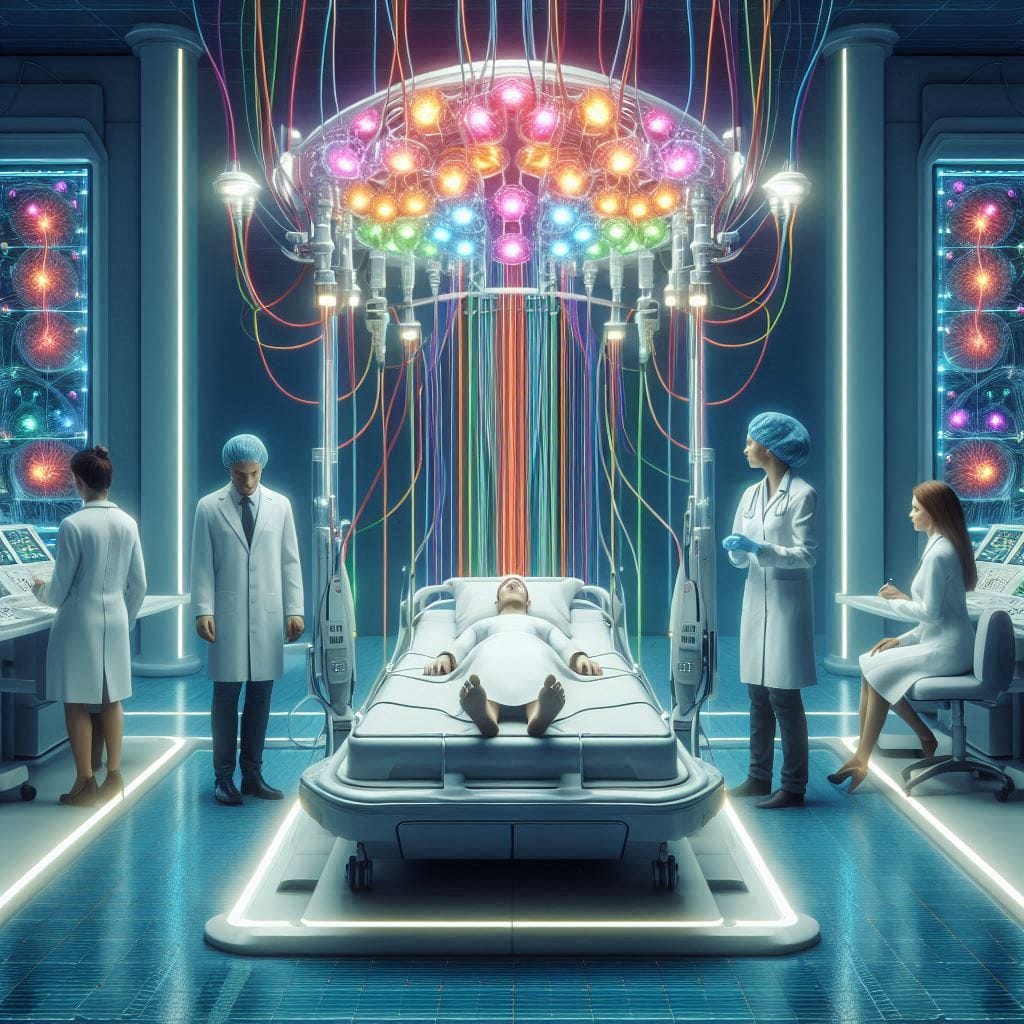
For optogenetics to work, light must be delivered to the neurons that have been modified to express opsins. This has traditionally been achieved using fiber-optic cables or LED arrays implanted in the brain. In animal models, these devices have been highly effective at delivering precise light pulses to specific brain regions. However, adapting these devices for use in humans presents several challenges.
One of the main challenges is minimizing the invasiveness of the devices. In rodents, fiber-optic cables are often permanently implanted in the skull, but this is not a practical solution for human patients. Researchers are working on developing smaller, more flexible devices that can be implanted with minimal impact on brain tissue. Advances in flexible electronics and wireless technology have shown promise in this area, to create implantable devices that can be controlled remotely and do not require frequent maintenance.

Another challenge is ensuring that the devices can deliver light to the appropriate brain regions without causing damage to surrounding tissue. This is particularly important in humans, where the risk of infection, bleeding, or scarring from invasive procedures is higher than in animal models. Researchers are exploring the use of new materials, such as biocompatible polymers and hydrogels, to create devices that are both effective and safe for long-term use in humans.
Despite these challenges, significant progress has been made in the development of optogenetic devices for humans. Several companies and research institutions are actively working on designing the next generation of optogenetic tools, with a focus on improving safety, efficacy, and patient comfort. These devices will be crucial for the successful translation of optogenetics therapy from the lab to the clinic.
Safety, Regulatory, and Ethical Considerations
The use of optogenetics in humans raises important safety, regulatory, and ethical questions. Ensuring the safety of patients is the top priority, particularly when dealing with invasive procedures such as brain implants and gene therapies. Clinical trials for optogenetics therapy must adhere to strict safety protocols, including rigorous testing of viral vectors, opsins, and implantable devices.
Regulatory approval for optogenetic therapies will likely be a complex and lengthy process. In addition to the challenges associated with gene therapy, optogenetics involves the use of light-based technologies and implantable devices, both of which must meet stringent safety and efficacy standards. Regulatory agencies such as the FDA will play a key role in determining when and how optogenetics in humans can be used in clinical settings.
Ethical considerations are also a significant factor in the development of optogenetic therapies. The potential for genetic modification of human cells raises concerns about the long-term effects of these treatments, particularly if they are used in children or individuals with genetic disorders. There is also the question of access to these therapies, as they may be expensive and not widely available to all patients.
Future Directions
Looking to the future, several trends could accelerate the development of optogenetics therapy for humans. One promising area of research is capsid engineering, which involves modifying the outer shell of viral vectors to improve their efficiency and specificity in delivering opsins to target cells. Advances in vector delivery methods, such as the use of synthetic nanoparticles or non-viral delivery systems, could also make optogenetics in humans safer and more effective.
Collaboration between academia and industry will be essential for advancing optogenetic gene therapy advancements. By working together, researchers and biotech companies can develop new tools and technologies that will make optogenetic therapies more accessible and affordable. There is also growing interest in using optogenetics to treat non-neurological conditions, such as heart disease or diabetes, by targeting specific cells in other organ systems.
Conclusion
In conclusion, optogenetics in humans holds immense potential for revolutionizing the treatment of neurological disorders. From vision restoration to Parkinson’s disease, the ability to precisely control neural activity with light offers a new approach to therapy that could be more effective and targeted than current treatments. However, significant challenges remain, including technical barriers, ethical concerns, and regulatory hurdles. As research continues to advance, the promise of optogenetics therapy may soon become a reality, offering new hope for patients suffering from debilitating conditions.
Further Reading on Cutting-Edge Technologies in Healthcare and Human Enhancement:
- Lab on Chip Technology: Dive into the world of miniaturized lab systems that promise to revolutionize diagnostics, drug development, and personalized medicine. Explore the future of healthcare with this breakthrough technology. Read more about Lab on Chip Technology here.
- The Future of Cyborg Enhancements: Discover how advancements in human augmentation, from neuroprosthetics to biomechanical enhancements, are bringing us closer to a cyborg future. Learn more about The Future of Cyborg Enhancements.
- Electronic Skin: Learn how ultra-thin, flexible electronic skin is enabling innovations in health monitoring, robotics, and prosthetics, offering a future where sensors seamlessly integrate with the human body. Explore the potential of Electronic Skin.
- Augmented Reality in Healthcare: Explore how augmented reality (AR) is transforming medical training, surgeries, and patient care by overlaying digital information onto the physical world. Discover more about Augmented Reality in Healthcare.