🧬 Introduction: A Radioactive Revolution in Cancer Treatment
“70% of trial patients saw tumor marker levels drop by half—with almost no side effects.”
This isn’t a headline from the future. It’s the outcome of the groundbreaking VIOLET trial, a clinical study testing a powerful new radioactive isotope: Terbium-161.
Developed by scientists at Peter MacCallum Cancer Centre in Australia, in collaboration with Isotopia Molecular Imaging (Israel), Terbium-161 is emerging as a game-changer in nuclear cancer therapy. Unlike conventional treatments that often affect healthy tissues along with tumors, this novel therapy uses highly targeted radiation to precisely destroy prostate cancer cells, while sparing surrounding tissues.
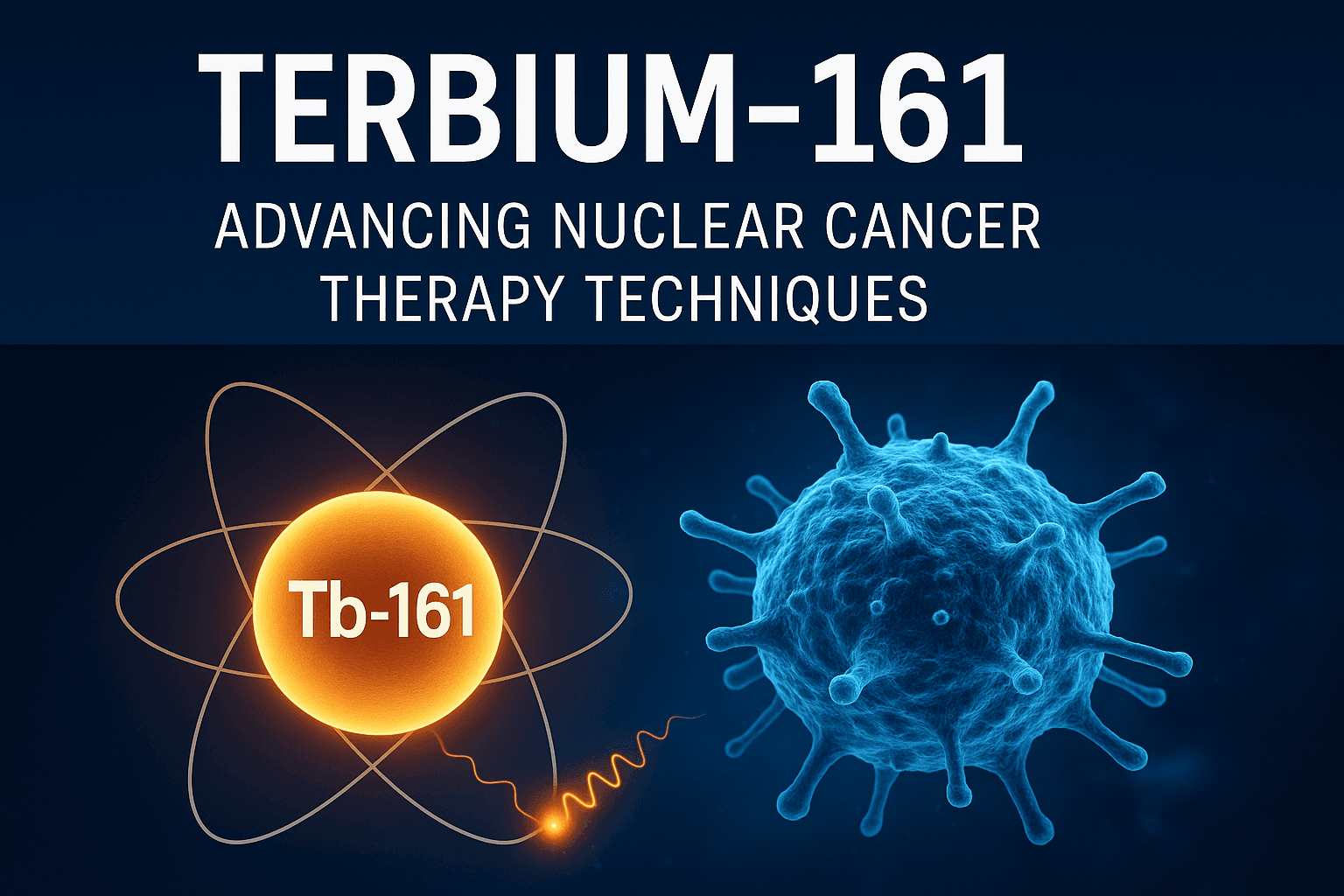
What sets Terbium-161 apart is its unique emission profile, which includes both beta particles and short-range Auger electrons. This dual-mode action enables more localized and lethal damage to cancer cells, offering superior therapeutic precision compared to widely-used isotopes like Lutetium-177.
The early success of the VIOLET trial—where nearly 7 in 10 participants experienced a 50%+ reduction in PSA (prostate-specific antigen) levels—signals a major step forward in the fight against cancer. And perhaps more importantly, these effects were achieved with minimal side effects, addressing a long-standing challenge in oncology: balancing efficacy with safety.
In this blog, we’ll explore:
- What makes Terbium-161 so revolutionary
- How it compares to traditional isotopes like Lutetium-177
- The science behind its precise targeting
- And what the future holds for nuclear cancer therapy using this next-gen isotope
🔬 What Is Terbium-161? The Science Behind the Isotope
Terbium-161 is a radioactive isotope belonging to the lanthanide group—a family of rare earth elements often used in advanced electronics and nuclear medicine. In recent years, it has gained attention as a promising nuclear isotope for cancer therapy, particularly in targeted treatments like prostate cancer.
What makes Terbium-161 especially valuable in oncology is its ideal physical half-life of approximately 6.9 days. It offers an ideal compromise—lasting just long enough to effectively target and damage cancer cells, while decaying quickly enough to minimize extended radiation exposure in the patient.
☢️ Dual-Mode Radiation: Why It’s a Precision Tool
Unlike traditional isotopes such as Lutetium-177, which primarily emit beta particles, Terbium-161 also releases Auger electrons—ultra-low energy particles with very short penetration depths (nanometers). This combination allows it to:
- Deliver broad tissue-level radiation via beta particles
- Administer cell-by-cell or even DNA-level damage via Auger electrons
This dual radiation profile makes Terbium-161 exceptionally lethal to targeted tumor cells, especially small-volume or micrometastatic disease, while minimizing collateral damage to healthy tissue.
Additionally, Terbium-161 can be paired with ligands like PSMA-617 that guide it specifically to cancer cells, making it a powerful tool for personalized nuclear medicine.
🧬 How Terbium-161 Targets Cancer Cells
Terbium-161 plays a central role in an advanced form of treatment called targeted radionuclide therapy (TRT)—a method that combines nuclear physics with precision oncology. This technique is transforming how we approach aggressive tumors like prostate cancer, especially when traditional therapies fall short.
🎯 What Is Targeted Radionuclide Therapy?
Targeted radionuclide therapy involves attaching a radioactive isotope (such as Terbium-161) to a molecule that seeks out specific cancer cells. This molecule is often a ligand or antibody that binds to markers uniquely expressed on the surface of tumor cells.
In the case of terbium-161 prostate cancer treatment, the isotope is commonly paired with PSMA-617—a molecule designed to bind with Prostate-Specific Membrane Antigen (PSMA), a protein found in high levels on prostate cancer cells.
Here’s how the process works:
- Injection: The radioactive compound (Terbium-161 + PSMA-617) is injected into the bloodstream.
- Targeting: PSMA-617 acts like a GPS, guiding the isotope directly to prostate cancer cells.
- Radiation delivery: Once bound, Terbium-161 emits radiation that destroys the cancer cell from within.
Unlike traditional radiation therapy, which affects both healthy and diseased tissue, TRT ensures highly selective cell killing, minimizing side effects.
⚛️ Why Terbium-161 Is So Effective at Cellular Destruction
What sets Terbium-161 apart from other isotopes is its ability to emit both beta particles and Auger electrons—a combination that maximizes damage at the cellular level.
🔹 Beta Particles:
- These particles have moderate penetration, enabling them to damage not only the targeted cell but also neighboring tumor cells.
- This is beneficial when treating larger tumors or clustered metastases.
🔹 Auger Electrons:
- These extremely low-energy electrons travel just a few nanometers—about the width of DNA strands.
- When emitted near or inside the cell nucleus, Auger electrons cause direct double-strand breaks in DNA, making them highly lethal to cancer cells.
- Crucially, their short range means healthy neighboring cells are largely spared, drastically reducing systemic toxicity.
This dual-damage mechanism gives Terbium-161 the unique ability to target:
- Microscopic tumors
- Residual cancer cells post-surgery
- Hard-to-reach metastases
🧬 The Future of Terbium-161 Prostate Cancer Therapy
Early results, such as those from the VIOLET trial, show that Terbium-161 prostate cancer therapy could outperform existing standards like Lutetium-177, especially in patients with advanced or resistant forms of cancer.
By delivering precision-guided, cellular-level destruction, Terbium-161 represents the next generation of nuclear medicine, offering hope where chemotherapy and external radiation often fail.
🧪 VIOLET Trial Results: Clinical Evidence of Success
In the rapidly evolving field of prostate cancer nuclear therapy, the VIOLET trial has emerged as a breakthrough study, showcasing the therapeutic promise of Terbium-161. Conducted by Peter MacCallum Cancer Centre in collaboration with Isotopia Molecular Imaging, the trial evaluated the safety and efficacy of Terbium-161 in patients with advanced metastatic prostate cancer.
📊 Remarkable Outcomes from the VIOLET Trial
The headline result from the VIOLET trial is both striking and hopeful:
🔬 70% of participants experienced a reduction of at least 50% in PSA (prostate-specific antigen) levels — a widely used biomarker for monitoring prostate cancer progression.
This level of response is significant, especially in patients who had already undergone multiple prior lines of treatment, including hormone therapy, chemotherapy, or even Lutetium-177 radionuclide therapy.
Safety was another strong point. Patients generally responded well to the treatment, experiencing only mild side effects with few complications. Unlike traditional chemotherapy or even some forms of radiation therapy, Terbium-161 did not cause severe systemic toxicity, offering patients a gentler yet effective option.
⚖️ Terbium-161 vs Lutetium-177: A Superior Successor?
While Lutetium-177-PSMA therapy is currently used in many cancer centers, Terbium-161 appears poised to become a more targeted and potent alternative. Here’s why:
| Feature | Terbium-161 | Lutetium-177 |
|---|---|---|
| Radiation Types | Beta + Auger electrons | Beta only |
| DNA-level damage | High (due to Auger electrons) | Moderate |
| Tissue penetration | More localized, ultra-precise | Broader but less targeted |
| Early trial outcomes | 70% PSA drop ≥50% (VIOLET trial) | ~46–50% PSA drop (typical in trials) |
The presence of Auger electrons in Terbium-161 leads to enhanced intracellular DNA damage, resulting in more effective tumor control—especially for micrometastases and resistant tumors.
💬 Real Voices from the Trial
Though full participant interviews are not widely published yet, one of the lead researchers from Peter MacCallum, Dr. Michael Hofman, noted in a public statement:
“Terbium-161 represents a major leap in the precision of radiopharmaceutical therapy. The dual emission allows us to deliver more focused treatment to the cancer site while minimizing toxicity.”
This underscores the paradigm-shifting nature of the VIOLET trial: a new isotope offering both better outcomes and fewer side effects.
⚖️ Terbium-161 vs Lutetium-177: Why It Matters
As nuclear medicine continues to reshape cancer treatment, two key players have emerged in the field of prostate cancer radiopharmaceuticals: Terbium-161 and Lutetium-177. Both isotopes are used in targeted radionuclide therapy, but their physical and biological properties differ in ways that may have significant clinical implications.
🧪 Side-by-Side Comparison: Terbium vs. Lutetium-177
Let’s compare the two isotopes across the features that matter most for therapeutic precision, safety, and efficacy:
| Feature | Terbium-161 | Lutetium-177 |
|---|---|---|
| Half-Life | ~6.9 days | ~6.7 days |
| Radiation Type | Beta particles + Auger electrons | Beta particles only |
| Damage Precision | Very high (nuclear/sub-cellular level) | Moderate (affects nearby healthy tissue) |
| Tissue Penetration | Short (Auger electrons cause local damage) | Longer (risk to surrounding cells) |
| Effectiveness | Higher (70% PSA drop in VIOLET trial) | Effective, but with limited penetration |
| Theranostic Pairing | Can be paired with PSMA-617 (therapy + imaging) | Commonly paired with PSMA-617 too |
🎯 Why Terbium-161 Could Be the Next-Gen Standard
While Lutetium-177 has become the backbone of prostate cancer nuclear therapy in recent years, the emergence of Terbium-161 is prompting researchers and oncologists to rethink what’s possible.
The key advantage of Terbium-161 lies in its dual emission profile:
- Beta particles provide deep tissue penetration for macroscopic tumor destruction.
- Auger electrons deliver pinpoint sub-cellular DNA damage, especially potent for micrometastases or residual cancer cells that evade conventional radiation.
This translates to greater tumoricidal efficiency with lower collateral damage, a combination that positions Terbium-161 as a potential next-generation radiopharmaceutical—not just for prostate cancer, but possibly for other solid tumors as well.
Moreover, its nearly identical half-life to Lutetium-177 allows for easy integration into existing treatment protocols and radiopharmacy infrastructure—making the transition to Terbium-161 both clinically impactful and logistically feasible.
✅ Bottom line: When comparing Terbium-161 to Lutetium-177, Terbium shows greater precision, enhanced cancer cell destruction, and reduced side effects—positioning it as a potential game-changer in prostate cancer radiopharmaceutical treatment.
🚀 Future Applications Beyond Prostate Cancer
While Terbium-161 has already shown exceptional promise in the treatment of prostate cancer, its unique characteristics position it for far broader impact. The future of nuclear medicine innovation may be defined by this single isotope, as research efforts expand its use into other cancer types that are notoriously difficult to treat.
🌐 Targeting More Than Just Prostate Cancer
Thanks to its dual-mode radiation (beta particles + Auger electrons) and compatibility with a wide variety of tumor-targeting ligands, Terbium-161 holds potential for treating a range of solid tumors beyond prostate cancer. Ongoing research is exploring its use in:
- 🧠 Neuroendocrine Tumors (NETs)
- These rare but aggressive cancers often resist traditional therapies.
- Terbium-161 could be paired with somatostatin analogs to specifically target neuroendocrine cells.
- The short-range Auger emissions may offer improved control over micrometastases.
- 🩺 Breast Cancer
- Certain subtypes of breast cancer (e.g., HER2-positive or hormone-receptor-positive) may be suitable for antibody-linked radiopharmaceuticals.
- Terbium-161 could be attached to HER2-targeting antibodies for highly focused treatment with minimal systemic toxicity.
- 🩻 Pancreatic Cancer
- Known for being hard to detect early and resistant to chemotherapy.
- Targeted radionuclide therapy using Terbium-161 may offer localized tumor eradication without harming surrounding pancreatic tissue, which is highly sensitive.
⚠️ Challenges to Overcome
Despite the optimism around the future of Terbium-161, several barriers must be addressed before it becomes a mainstream clinical option:
🏭 1. Production Scalability
- Terbium-161 is typically produced in nuclear reactors using neutron irradiation.
- Scaling up production to meet clinical demand—while maintaining purity and safety—requires international cooperation and infrastructure expansion.
📝 2. Regulatory Approvals
- Each country’s health regulatory authority (e.g., FDA, EMA, TGA) has different timelines and requirements.
- Full phase 3 trials, long-term safety tracking, and theranostic validation will be essential.
🌍 3. Global Accessibility
- Low- and middle-income countries may struggle to access nuclear isotopes due to infrastructure, cost, or import/export restrictions.
- Ensuring equitable distribution will be critical for the global impact of Terbium-161.
💡 With its sub-cellular precision and wide applicability, Terbium-161 has the potential to revolutionize not just prostate cancer care—but the entire landscape of personalized nuclear oncology.
⚠️ Ethical, Safety, and Regulatory Considerations
As Terbium-161 cancer therapies move from clinical trials to wider application, it’s crucial to address the ethical, safety, and regulatory frameworks that will govern their use. The nature of radioactive materials, while medically beneficial, demands strict controls to protect patients, healthcare workers, and the environment.
🧪 Safe Handling of Isotopes
Because Terbium-161 is a radioactive isotope, it must be handled in specialized nuclear medicine facilities with:
- Lead shielding
- Trained radiopharmacists and nuclear technicians
- Strict transport and disposal protocols
Radiation exposure to medical staff must remain within international safety thresholds, and all use is typically monitored by dosimeters and audit logs.
📏 Dosage Control & Patient Eligibility
Accurate dosimetry—measuring and delivering the right radiation dose—is essential for:
- Maximizing tumor destruction
- Minimizing healthy tissue exposure
- Avoiding unnecessary long-term radiation side effects
Patient selection also plays a role. Individuals must:
- Exhibit PSMA expression or relevant cancer markers
- Pass renal, liver, and bone marrow function tests
- Undergo pre-treatment imaging to ensure target uptake of the isotope
🌍 Regulatory Oversight
Before Terbium-161 nuclear therapies become widespread, they must pass rigorous scrutiny by national and international regulatory agencies:
| Region | Regulatory Body | Role |
|---|---|---|
| Australia | TGA (Therapeutic Goods Administration) | Oversees radiopharmaceutical trials and drug registration |
| United States | FDA (Food and Drug Administration) | Approves new drugs, monitors trial safety, post-market surveillance |
| Europe | EMA (European Medicines Agency) | Coordinates EU-wide clinical evaluations and safety data |
These bodies assess:
- Clinical efficacy
- Manufacturing standards
- Long-term follow-up plans
♻️ Environmental Advantage: Short Half-Life
One unique safety and sustainability advantage of Terbium-161 is its relatively short half-life (~6.9 days). This means:
- Minimal radioactive waste remains after treatment
- Safer and more efficient waste disposal protocols
- Reduced risk to the public or environment in case of isotope mishandling
This property supports not just patient safety—but also ecological responsibility in the advancement of nuclear medicine.
🧬 Conclusion: A New Age of Radiotherapy
The story of Terbium-161 cancer treatment is still unfolding—but even now, it’s clear that this isotope represents a major leap forward in precision oncology.
By combining:
- Higher therapeutic precision through Auger electron emission
- Better clinical outcomes, such as improved PSA reduction rates
- Lower toxicity and environmental impact due to its physical profile
Terbium-161 is rapidly becoming a symbol of innovation in nuclear medicine.
Its versatility across tumor types, combined with its strong early trial results, point toward a future where cancer therapies are safer, smarter, and more effective than ever before.
💡 As clinical trials progress, Terbium-161 may soon redefine the way we fight cancer—from the inside out.
💡 Enjoying this deep dive into nuclear cancer therapy?
Don’t miss our other groundbreaking explorations in next-gen medicine:
-
🔬 Hydroxyapatite 2040: The Future of Limb and Tooth Regrowth – Discover how this bioactive material could redefine human regeneration.
-
🧪 Methylene Blue: Bridging Medicine and Future Technology – A surprising old dye making a comeback in neuroscience, anti-aging, and beyond.
-
🤖 The Nanobots Cancer Cure: A Revolutionary Progress – Explore how microscopic robots are being designed to target and destroy tumors at the cellular level.
Click the titles to explore more futuristic breakthroughs in healthcare.